Anterior abdominal wall
You will find in the submenu above topics relating to the abdominal wall.
Introduction
This section will explore the layers of fascia and muscles involved in forming the anterior abdominal wall and the rectus sheath
Fascia of the abdominal wall
Superficial fascia of the abdominal wall
Above the level of the umbilicus:
- a superficial fatty layer: a layer containing a variable amount of fat
Below the level of the umbilicus:
- Superficial fatty layer (Camper’s fascia)
- This is a poorly defined layer of fat under the skin. It has little structural integrity
- In males, Camper's fascia extends onto the penis and scrotum in the form of Dartos' Fascia.
- This is a well defined fibrous layer of tissue deeper to Camper's fascia
- The fibrous nature of the layer gives it good tensile strength
- It is attached to the deep fascia of thigh 2.5 cm below the inguinal ligament
- This stops urine reaching the thigh when bulbous urethra ruptures
- This stops an undescended testis from descending into the thigh
- Extends into perineum as Colles’ fascia.
- Colles’ fascia is attached to the perineal body, perineal membrane and laterally to the rami of the pubis and ischium.
Other fascia in the anterior abdominal wall:
- Investing fascia
- Layers of fascia that cover the external aspect of the anterior abdominal wall muscles.(external oblique, internal oblique and transversus abdominis)
- Endoabdominal fascia:
- a membranous sheet of fascia internal to all muscle groups.
- Can be named after the portion of muscle it associates with
- For example, the fascia lining the internal surface of the transversus abdominis muscle is called the transversalis fascia.
- Parietal Peritoneum:
Anterior abdominal wall muscles:
There are 4 muscles in the anterior abdominal wall. They are paired (4 on the right and 4 on the left)
| Muscle Name | Notes |
|---|---|
| Rectus Abdominis |
|
| External Oblique |
|
| Internal Oblique |
|
| Transversus Abdominis |
|
Rectus abdominis muscle:
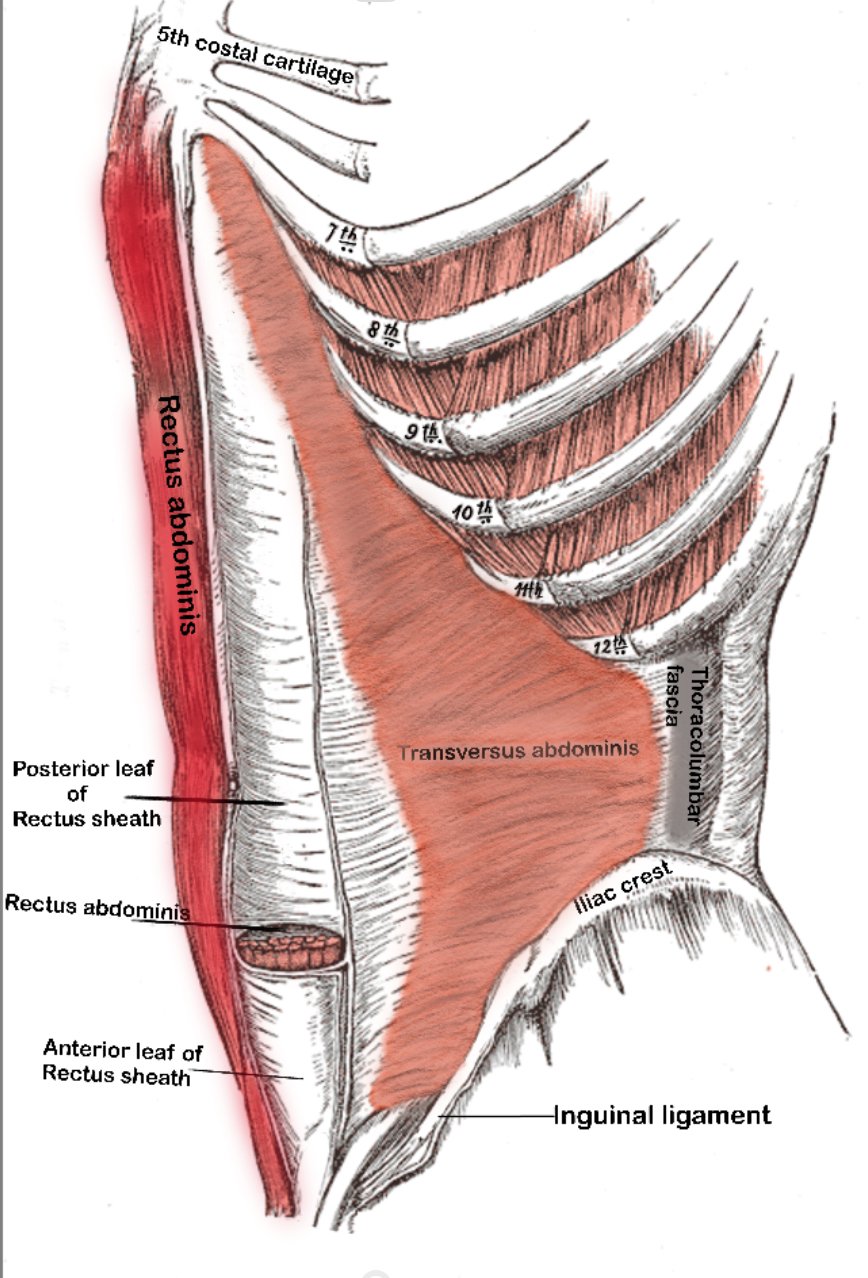
fig.2 Rectus Abdominis muscle
- Long strap-like muscle, extending the length of the abdominal wall.
- Enclosed in the rectus sheath
| Origin | 5th, 6th, 7th costal cartilages |
| Insertion | Pubic crest |
| Innervation | Lower six thoracic nerves (T6-T12) |
- The rectus abdominis has tendinous intersections along its course.
- The long muscle fibres are interrupted by these tendinous intersections allowing for increased contraction strength.
- The intersections attach to the anterior rectus sheath.
- This forms the appearance known as the "six pack".
- The number of intersections varies by genetics:
- Classically there are 3 intersections:
- Level of xyphoid
- Level of umbilicus
- Halfway between the 2 points
- Classically there are 3 intersections:
External oblique muscle:
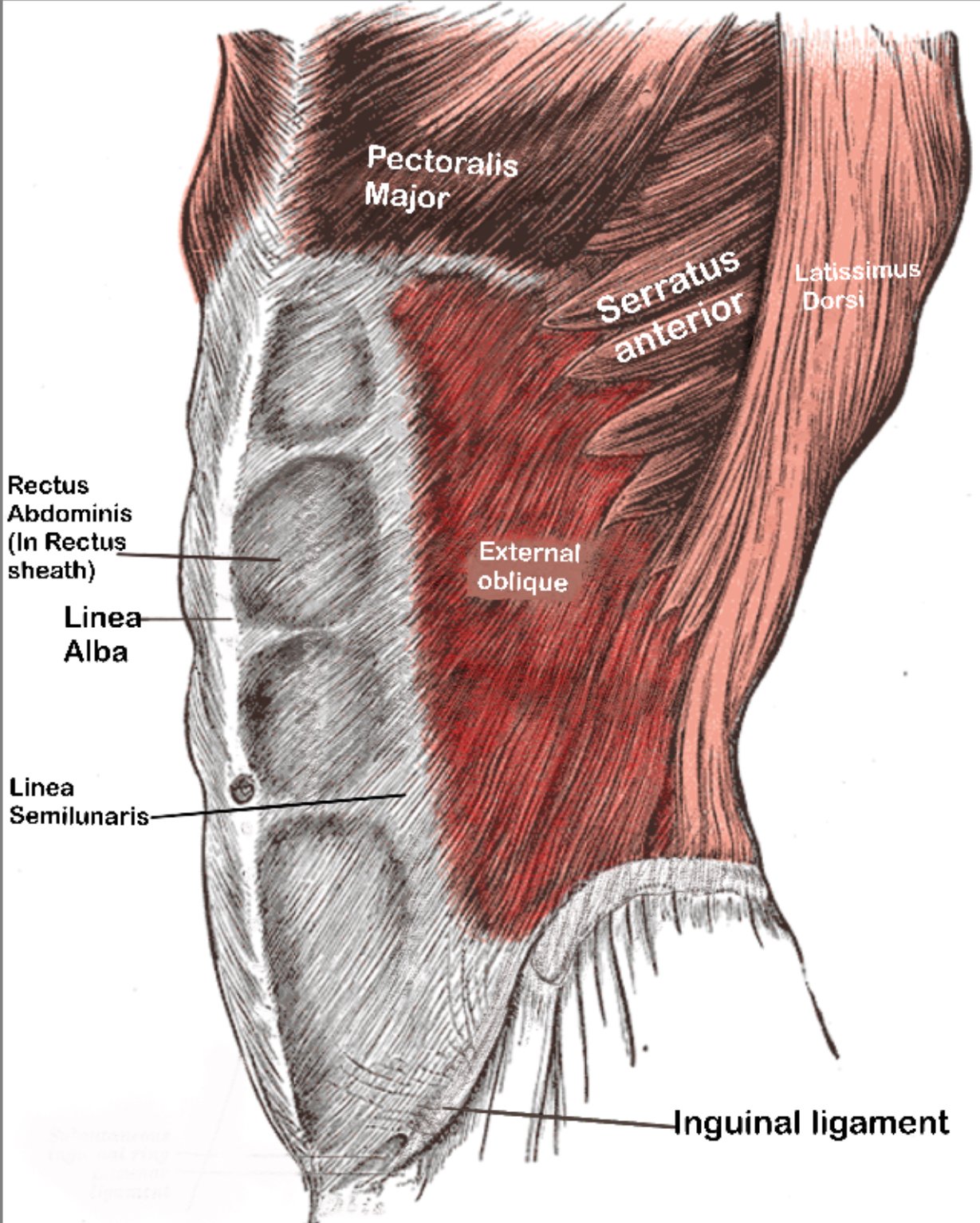
fig.2 External oblique muscle
- The most superficial sheet muscle.
- Its fibres pass inferomedially.
- The inferior margin is thickened forming the inguinal ligament.
- This spans between the anterior superior iliac spine (ASIS) and pubic tubercle.
| Origin | External surfaces of 5th–12th ribs |
| Insertion | Linea alba, pubic tubercle, ASIS and anterior half of iliac crest |
| Innervation | Anterior rami of lower 6 thoracic nerves and subcostal nerve |
Internal oblique muscle:
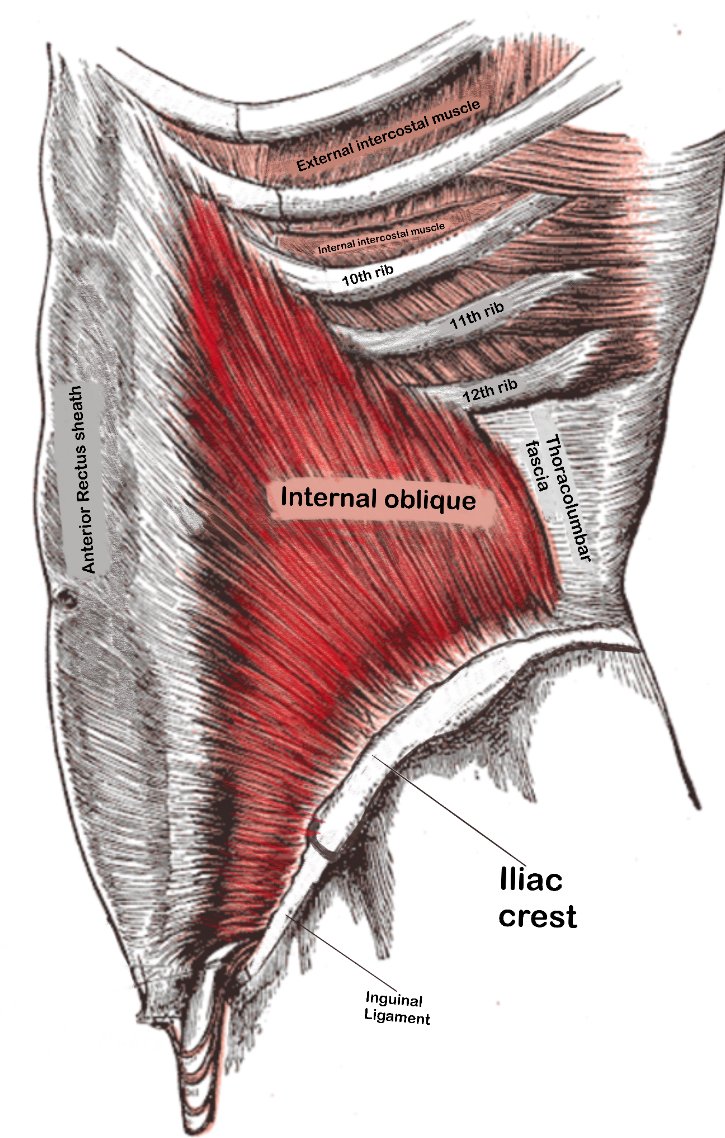
fig.3 Internal oblique muscle
- It is a broad sheet-like muscle located deep to the external oblique and superficial to the transversus abdominis.
- Fibres are arranged in a fan-like fashion.
- The superior fibres are perpendicular to fibres of external oblique.
- The inferior fibres are parallel to the external oblique (hand in pocket appearance).
| Origin | Thoracolumbar fascia posteriorly. Anterior 2/3 of the iliac crest laterally. |
| Insertion | Linea alba, inferior borders of lower 2 ribs, and pubis |
| Innervation | Lower sixth thoracic nerves and iliohypogastric and ilioinguinal nerves. |
Transversus abdominis
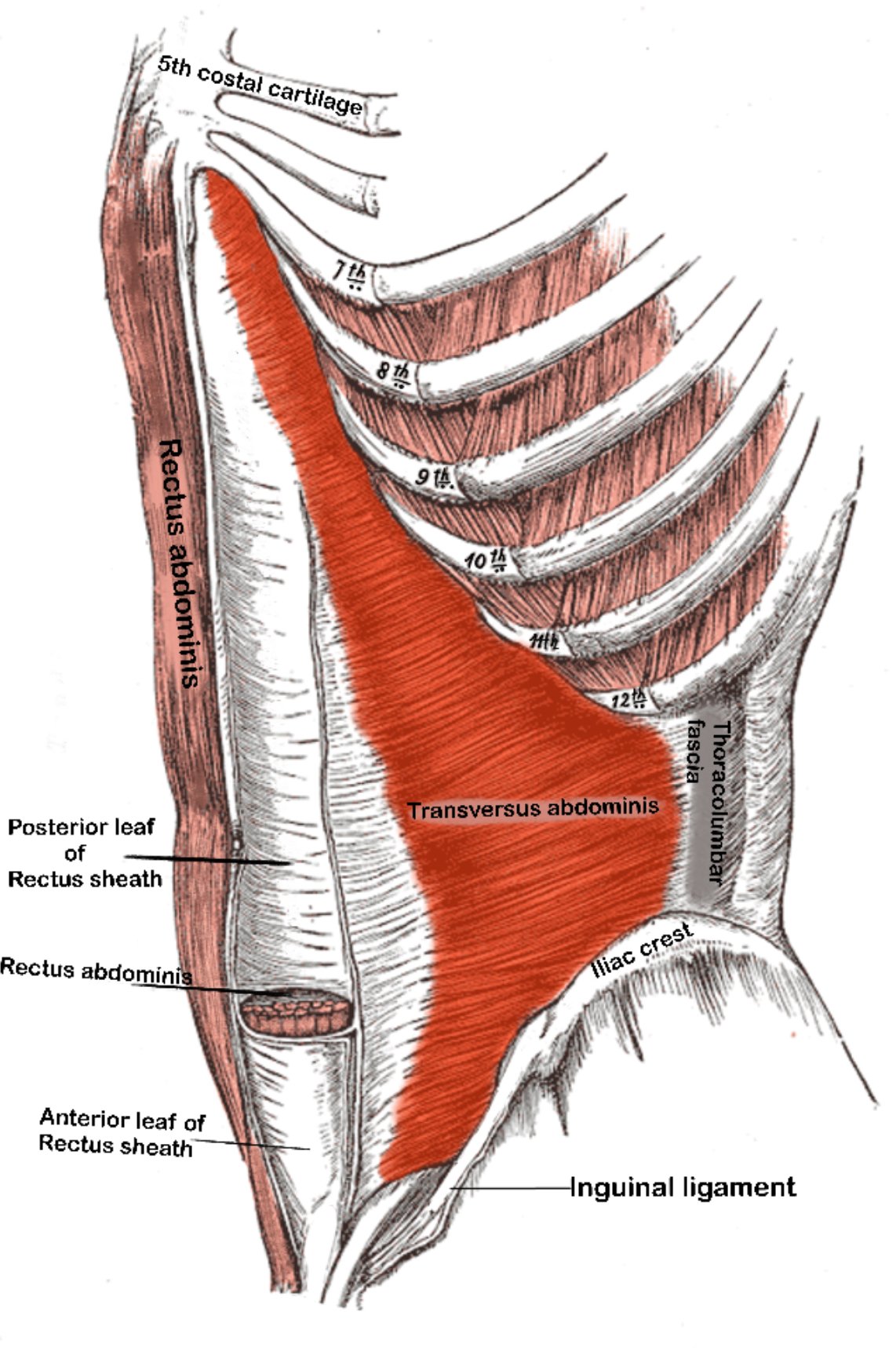
fig.4 Transversus abdominis muscle
The innermost of the 3 sheet muscles. Its fibres run horizontally.
| Origin |
|
| Insertion |
|
| Innervation | Lower sixth thoracic nerves and iliohypogastric and ilioinguinal nerves. |
Function of the anterior abdominal wall muscles:
- The muscles act to compress and support the abdominal viscera
- The muscles work together to flex and rotate the trunk and stabilise the pelvis.
Sensory supply of the anterior abdominal wall
Cutaneous innervation of the trunk:
Each nerve supplying the abdominal wall originates from the spinal cord and exits through the intervertebral foramen as a thoracoabdominal nerve (T7-T11), subcostal nerve (T12), or a branch from the lumbar plexus (L1).
Pathway and Branching:
Exiting the Spinal Cord
- The nerves leave the spinal cord at their respective levels, emerging from the spinal root.
- They begin their journey between the ribs (in the case of thoracic nerves) or directly into the abdominal region (for the subcostal and lumbar nerves).
Initial Branching
- As each nerve travels laterally, it divides into:
- Posterior Cutaneous Branch: Supplies the skin over the paraspinal region.
Further Lateral Course and Branching
- The main nerve then continues between the internal oblique and transversus abdominis (the transversus abdominis plane), where it divides further into:
- Lateral Cutaneous Branch: Emerges at the side of the abdomen, supplying sensation to the lateral aspect.
- Anterior Cutaneous Branch: Pierces the rectus abdominis to supply sensation along the midline.
Dermatomes of the anterior abdominal wall:
- The sensory supply (skin and parietal peritoneum) is carried by thoracic nerves:
- T10 anterior cutaneous branch: Supplies sensation around the umbilicus.
- T7-T9 anterior cutaneous branches: Cover areas above the umbilicus.
- T11 and T12 anterior cutaneous branches: Cover areas below the umbilicus.
- Iliohypogastric and Ilioinguinal Nerves (L1):
- Iliohypogastric nerve: Supplies sensation to the skin above the pubic region
- Ilioinguinal nerve: Supplies sensation to the groin area and inner thigh
Coverage Summary
- Posterior Cutaneous Branch: Supplies the back and paraspinal region.
- Lateral Cutaneous Branch: Supplies the side and lateral parts of the abdominal wall.
- Anterior Cutaneous Branch: Supplies the front of the abdominal wall along the midline.
Clinical relevance: Transversus abdominis (TAP block)
A Transversus Abdominis Plane (TAP) block is a regional anesthesia technique used to provide analgesia to the anterior abdominal wall by targeting the nerves that innervate it.
Anatomy of the TAP block:
- The goal is to anesthetize the lateral cutaneous and anterior cutaneous branches of T7-T12 and L1 by injecting local anaesthetic between the internal oblique and transversus abdominis.
Technique:
- Ultrasound-guided block: Local anaesthetic is injected into the plane between internal oblique and transversus abdominis muscles.
- Laparoscopic block:
- A needle is advanced to the correct plane under direct vision with a laparoscopic camera.
- If injected correctly, a Doyle’s bulge (a distinct bulge in the tissue plane) is seen.
- If injected too deep, a peritoneal bleb forms.
- Common injection sites:
- Subcostal injection lateral to rectus abdominis muscle border
- Anterior axillary line midway between iliac crest and costal margin
Midline Rectus Sheath:
- The 3 sheet muscles form a thick aponeurosis medially, enclosing the rectus abdominis muscle.
- The lateral boundary where the rectus abdominis meets the aponeuroses is the linea semilunaris.
- Medially, the aponeuroses join to form the linea alba.
- The linea alba has minimal blood supply, allowing rapid access to the abdomen (useful in surgical emergencies), but also slower healing.
Arcuate line:
- The halfway point between umbilicus and pubic symphysis.
- It is where the inferior epigastric vessels enter the rectus sheath.
- Below the arcuate line, all aponeuroses run anterior to the rectus abdominis, thinning the posterior wall and allowing vessels to pierce more easily.
| Muscle aponeurosis | Relation above the arcuate line | Relation below the arcuate line |
|---|---|---|
| External oblique | Anterior to rectus abdominis | Anterior to rectus abdominis |
| Internal oblique | Splits into anterior and posterior layers around rectus abdominis | All aponeurosis anterior to rectus abdominis |
| Transversus abdominis | Posterior to rectus abdominis | Anterior to rectus abdominis |

Above the Arcuate Line

Below the Arcuate Line
Because the aponeurosis is anterior below the arcuate line, the posterior sheath is thinner, creating a potential area of weakness where a Spigelian hernia can occur.
Contents of the rectus sheath:
- Rectus muscle
- Anastomosing superior and inferior epigastric vessels
- Lymphatics
- Nerves supplying muscle and overlying skin
Arteries of the anterior abdominal wall
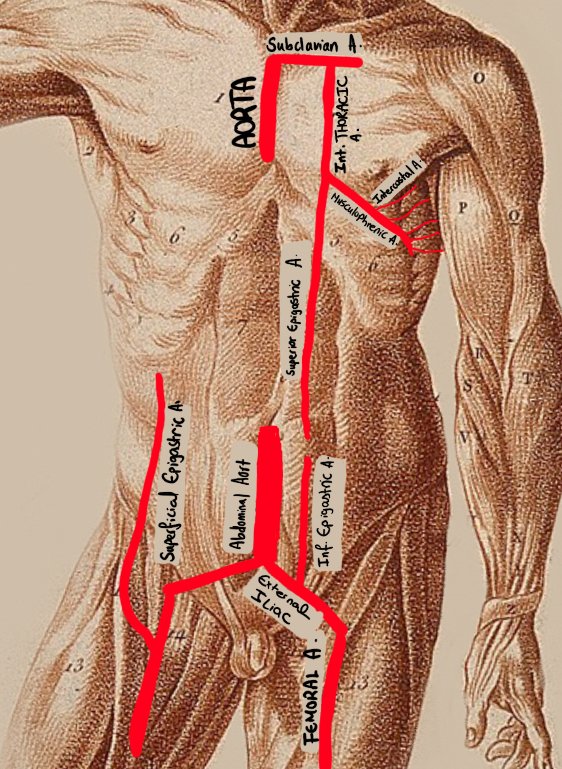
Anterior abdominal wall arterial supply
Internal thoracic artery
- Branch of subclavian artery
- Divides into 2 main branches
- Musculophrenic (supplies muscles and diaphragm)
- Runs along the costal margin
- Branches into intercostal arteries
- Superior epigastric artery
- Runs in the rectus sheath deep to rectus abdominis
- Anastomoses distally with the inferior epigastric
- Musculophrenic (supplies muscles and diaphragm)
Inferior epigastric artery
- Branch of the external iliac artery
- Runs superiorly, entering rectus sheath at the level of the arcuate line
- Runs deep to rectus abdominis in rectus sheath
- Anastomoses superiorly with the superior epigastric artery
Clinical relevance
During a laparoscopic appendicectomy, the proximal portion of this artery should be identified when inserting the left iliac fossa port to avoid injury.
Superficial epigastric artery
- Branch of the femoral artery
- Runs in superficial fascia towards umbilicus
Clinical relevance
Commonly encountered during open inguinal hernia repair. It is advised to ligate rather than cauterise to prevent hematomas.
Venous drainage of the anterior abdominal wall
Venous drainage largely follows the arteries. A key difference is the thoracoepigastric vein.
Thoracoepigastric vein
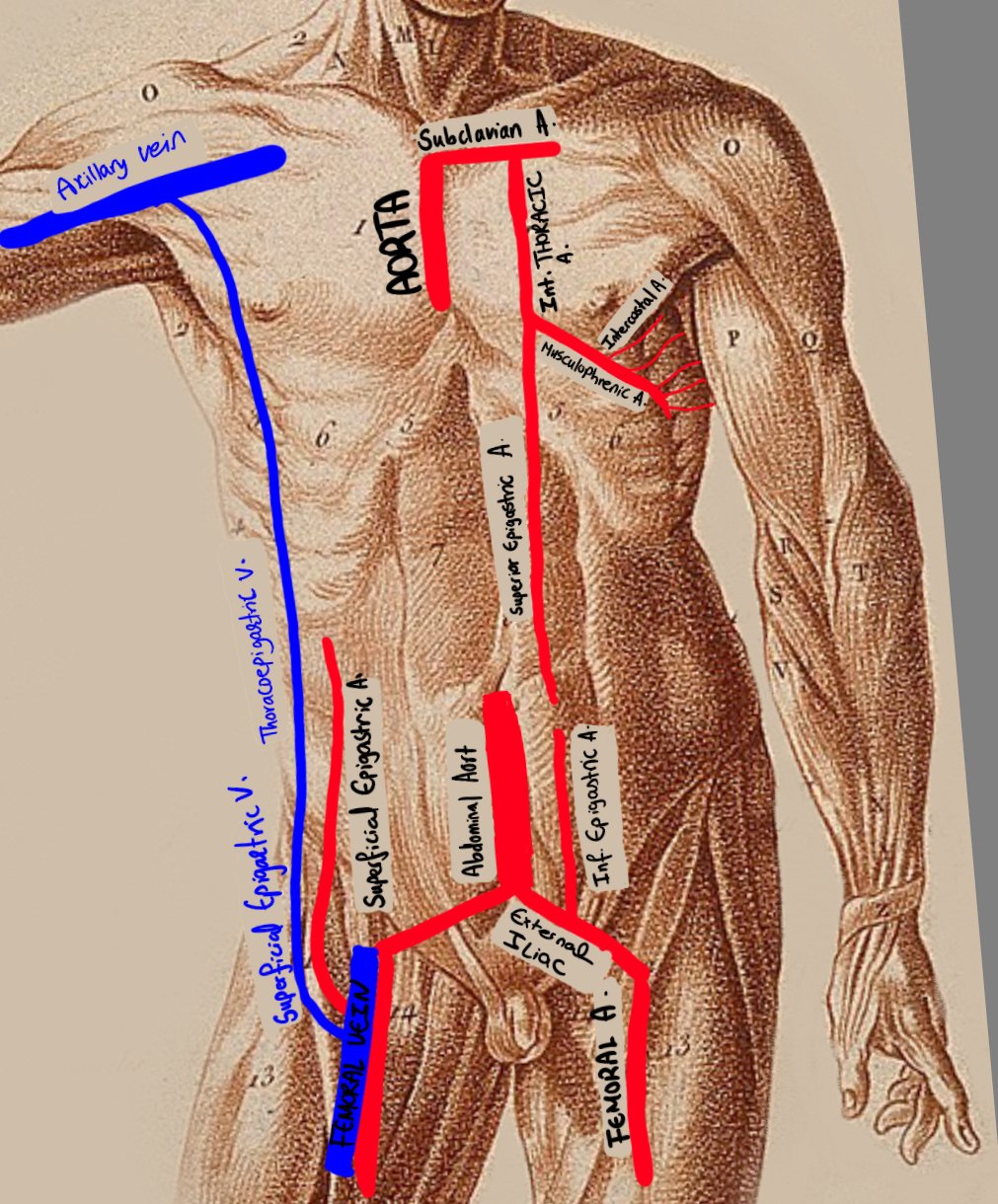
Anterior abdominal wall venous supply largely follows arterial supply. The thoracoepigastric vein (the exception) is depicted on the diagram.
This vein provides an indirect anastomosis between the IVC and SVC.
It is a branch of the superficial epigastric vein (branch of the femoral vein).
It anastomoses superiorly with the axillary vein which drains into the SVC, bypassing the IVC.
If the IVC is blocked, blood from the lower limb can still return to the heart via this route.
Route of bypass
Femoral vein
Superficial epigastric vein
Thoracoepigastric vein
SVC
Layers of the anterior abdominal wall
The layers of the abdominal wall differ in different parts of the abdominal wall.
A cut down through layers in the midline will reveal layers vastly different to a cut lateral to the rectus abdominis muscles.