Appendix
Anatomy Of The Appendix
What Is The Vermiform Appendix?
The vermiform appendix is a blind ended true diverticulum of the colon. It extends from the posteromedial aspect of the cecum, 2.5 cm inferior to the ileocecal valve, ending blindly in the right iliac fossa (RIF).
Explanation of the definition
True diverticulum?
- a diverticulum is a pouch or a sac extending from a hollow organ.
- it is considered a true diverticulum as its wall is made from all the layers that make up the colonic wall.
- A false diverticulum will only be made of mucosa/submucosa.
Vermiform
- worm like in appearance.
Location
- It arises from the posteromedial aspect of the cecum.
- The cecum is a pouch forming the first part of the colon.
- The appendix arises posteriorly (behind) and from the medial aspect of it.
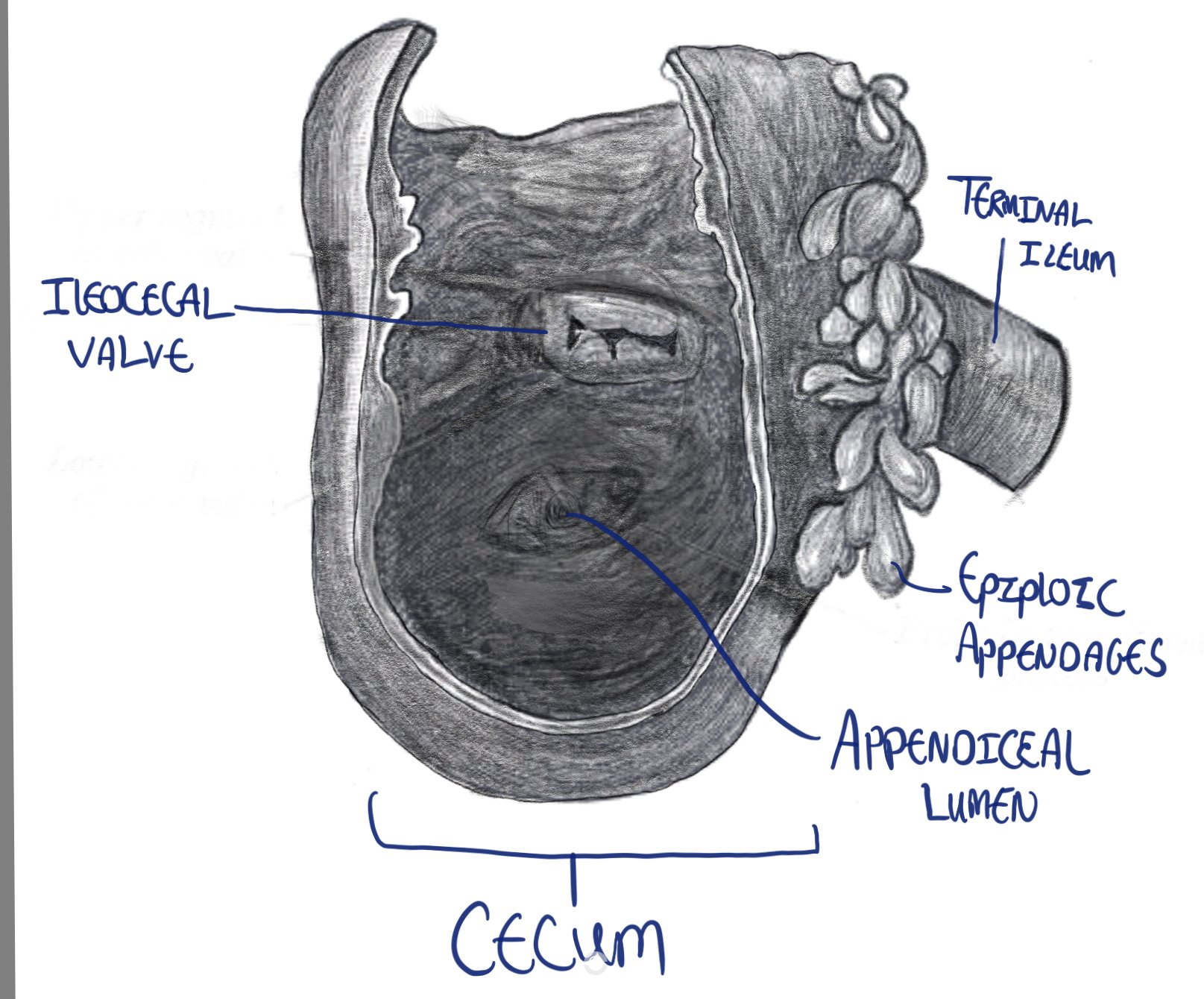
Drawing of the cecum, showing the ileocecal valve and appendiceal lumen.
Location Of The Appendix
A common question you might get asked by a senior when you scrub in for your first appendicectomy is “where would I find the appendix?”, and it’s a fair question as after all you can’t remove something if you don’t find it! You can answer this as follows:
- It’s in the region of the RIF (Right Iliac Fossa).
- Find the ascending colon, when you find it follow the taeniea coli proximally.
- Look for the part of the colon where the three taeniae converge.
- Voila! You should now find the appendix (unless it’s been removed or it’s in an abscess cavity surrounded by inflammation).

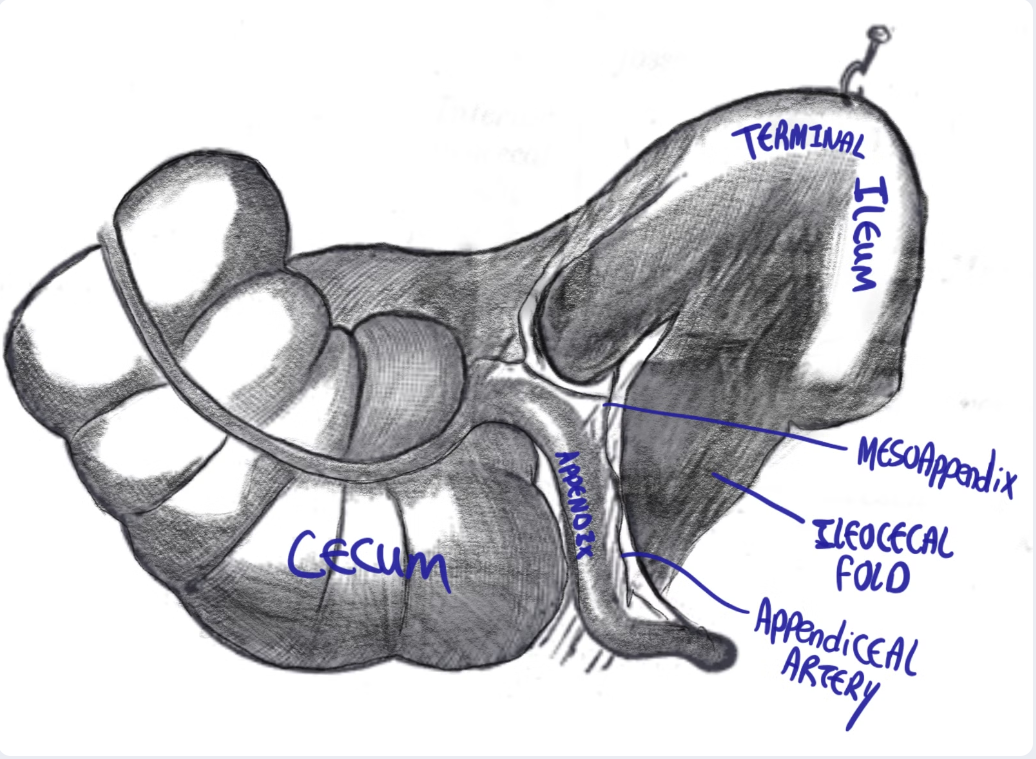
freehand drawing showing the cecum, terminal ileum, tinea coli <!!should be “taenia coli”!!>, haustra, appendix and ileocecal fold
Clinical relevance
To further complicate things, malrotation and nonrotation of gut can move the appendix to the left upper quadrant. This is why the surgical dictum dictates acute appendicitis should be in the top 3 differentials of acute abdominal pain regardless of location.
side note: what is taeniae coli?
- I am glad you asked!
- Taenia coli are 3x 8mm wide longitudinal muscles bands in the colon wall.
- They are parallel, and form a triple helix structure from the appendix to the sigmoid colon, where they coalesce.
Surface Anatomy: McBurney’s Point
McBurney’s Point Location
The base of the appendix classically lies at a point that lies 1/3 of the distance laterally on a line drawn between the umbilicus and the right ASIS (Anterior Superior Iliac Spine).

Diagram depicting the position of McBurney's point.
Position Of The Appendix
This refers to the position of the free-end (or tip) of the appendix.
- The position of the appendicular orifice in the cecum (base) is consistent but the appendicular tip position is highly variable.
- This variability is due to the mobile nature of the surrounding bowel and the wide variation in length of appendix
- The position of the appendix can be in one of 7 positions, depending on the relationship of the appendix to the surrounding structures.
- The positions can be thought of the numbers on a clock face.
- Most common position is retrocecal (65% of the time).

a diagram showing different common positions of the appendix.
Positions of the appendix in relation to the terminal ileum
The appendix can be found in various positions relative to the ileum. These positions are typically described using a clock face analogy for easy reference:
Post ileal
This position is behind the ileum, corresponding to the 1 or 2 o’clock position.
Pre-ileal
In this position, the appendix is located in front of the ileum, also at the 1 or 2 o’clock position.
Para-ileal
Here, the appendix runs parallel to the Terminal ileum, represented by the 3 o’clock position.
Pelvic
In this position, the appendix extends inferiorly into the pelvis, corresponding to the 6 o’clock position.
Positions of the appendix in relation to the cecum
Retrocecal
This is the most common position, occurring in 65% of cases. The appendix sits posterior to the cecum, usually extending upwards behind it. It is found at the 11 o’clock position.
Subcecal
This position is on the inferior aspect of the cecum (not posterior to it!). It is located at the 8 o’clock position and occurs in 31% of cases.
Paracecal
In this position, the appendix is situated alongside the lateral border of the cecum, at the 10 o’clock position.
Clinical relevance
patient with appendicitis, with a retrocecal appendix can present with leukocytes and blood in urine. This happens due to irritation of the ureter by the surrounding inflammation. A positive urine dip does not always mean stones or UTI! Use your clinical judgement!!
Size Of The Appendix
Length of the appendix:
- Average length is 8-10cm.
- Range is 2-20cm.
- Larger size not indicative of pathology.
Diameter
- a diameter of over 6mm can be considered distended and potentially pathological
Wall thickness
- A wall thicker than 3mm can be considered thickened and potentially pathological.
Size on Ultrasound scanning:
- Ultrasonographic imaging can be used to asses <!!should be “assess”!!> the appendix, size is an important criteria in diagnosing appendicitis.
- The appendix is measured at the thickest point in the cross sectional image.
Measurements:
- MOD (maximal outer diameter) (over 6mm pathological)
- This refers to the diameter of the appendix.
- Defined on ultrasound as the distance between the outer hyperechoic borders of the appendix.
- MMT (Maximal mural thickness) (over 3mm pathological)
- The thickness of the appendiceal wall.
- Was defined as the distance from the hyperechoic luminal interface to the outer hyperechoic border.
Appendiceal mesentery (AKA mesoappendix)
- it is a fold of peritoneum around the vermiform appendix.
- Contains the appendiceal artery and vein.
Attachments:
proximal attachment:
- AKA bloodless fold of Treves.
- This is a fold of mesentery found in the angle between the antimesenteric border of the ileum and the cecum.
- it is named after Sir Frederick Treves, a surgeon in a London hospital in the early 1900s, who was renowned for operating on King Edward the VII for appendicitis.
- Despite its name, the bloodless fold of Treves is rarely actually bloodless, and usually contains a vessel!
- Appearances are very similar to the colon and cecum
- layers
- Mucosa: made of columnar epithelim <!!should be “epithelium”!!> with goblet and endocrine cells.
- submucosa: contains blood vessels, lymph nodes and connective tissue
- muscularis: inner circular muscular layer, lacks tinea <!!should be “taenia”!!>
- serosa: outer layer of visceral peritoneum.
- Distinct features (relates to the supposed immune function of the appendix)
- More presence of lymph follicles and parafollicular tissue in the connective tissue layer of the mucosa (lamina propria)
- M cells: microfold cells are foind <!!should be “found”!!> in the epithelium and can sample antigens and pathogens from the intestinal lumen.
- lacks tinea <!!should be “taeniae”!!>: outer muscle later <!!should be “layer”!!> is regular.
- The appendiceal lumen narrows with age and can become completely obliterated in the elderly, which is why appendicitis is less common in older adults.
- The narrowing and potential obliteration of the appendiceal lumen in older adults is directly related to the incidence of appendicitis in this age group. Specifically, appendicitis becomes less common in older adults. This reduced frequency of appendicitis in the elderly population can be attributed, at least in part, to these age-related changes in the appendix’s internal structure.
- Appendiceal artery: Branch of the ileocolic artery
- The appendix is supplied by a single artery.
- In appendicitis, due to inflammation, the intraluminal pressure will exceed the perfusion pressure resulting in ischemic injury. This ischaemia predisposes to perforation.
- On the other hand the gallbladder is supplied by the cystic artery AND the liver bed, so even if the cystic artery is compromised, it will still get some blood supply through the liver bed.
- Follows the venous drainage
- Drains into the lymph nodes in the mesoappendix and later into the ileocolic lymph nodes (surrounding ileocolic artery)
- superior mesenteric plexus
- carried on the sympathetic nerve fibres that enter the spinal cord at T10
- The dermatome for this nerve root is T10.
- Pain from appendicitis typically presents as vague paraumbilical pain that localizes to the right iliac fossa (RIF). This is sometimes classically described as migratory central to RIF pain.
- Pain at the paraumbilicus: Felt here because the appendix is supplied by sensory fibers that enter the spinal cord at the level of T10 (the T10 dermatome corresponds to the umbilicus).
- Pain at the RIF: This pain occurs when the inflammation worsens and starts irritating the parietal peritoneum of the abdominal wall.
ileocaecal fold:
Distal attachment: extends to the tip of the appendix.
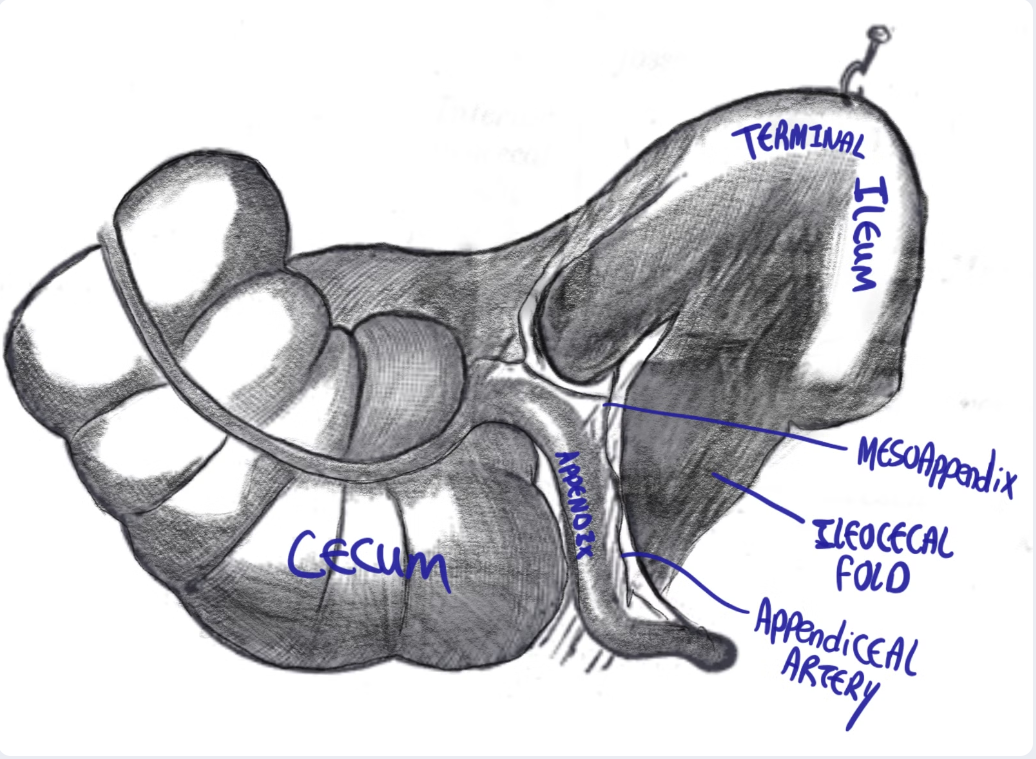
freehand drawing showing the cecum, terminal ileum, tinea coli <!!should be “taenia coli”!!>, haustra, appendix and ileocecal fold
Appendiceal histology
Lumen of the appendix
Blood Supply And Lymph Drainage
Arterial Supply
Abdominal aorta
Superior mesenteric artery (SMA)
ileocolic artery
appendiceal artery
Location: Contained in the mesoappendix
Characteristics: End artery, usually solely supplies the appendix
Remember: The appendix is a structure of the midgut, so it’s supplied by a branch of the SMA.
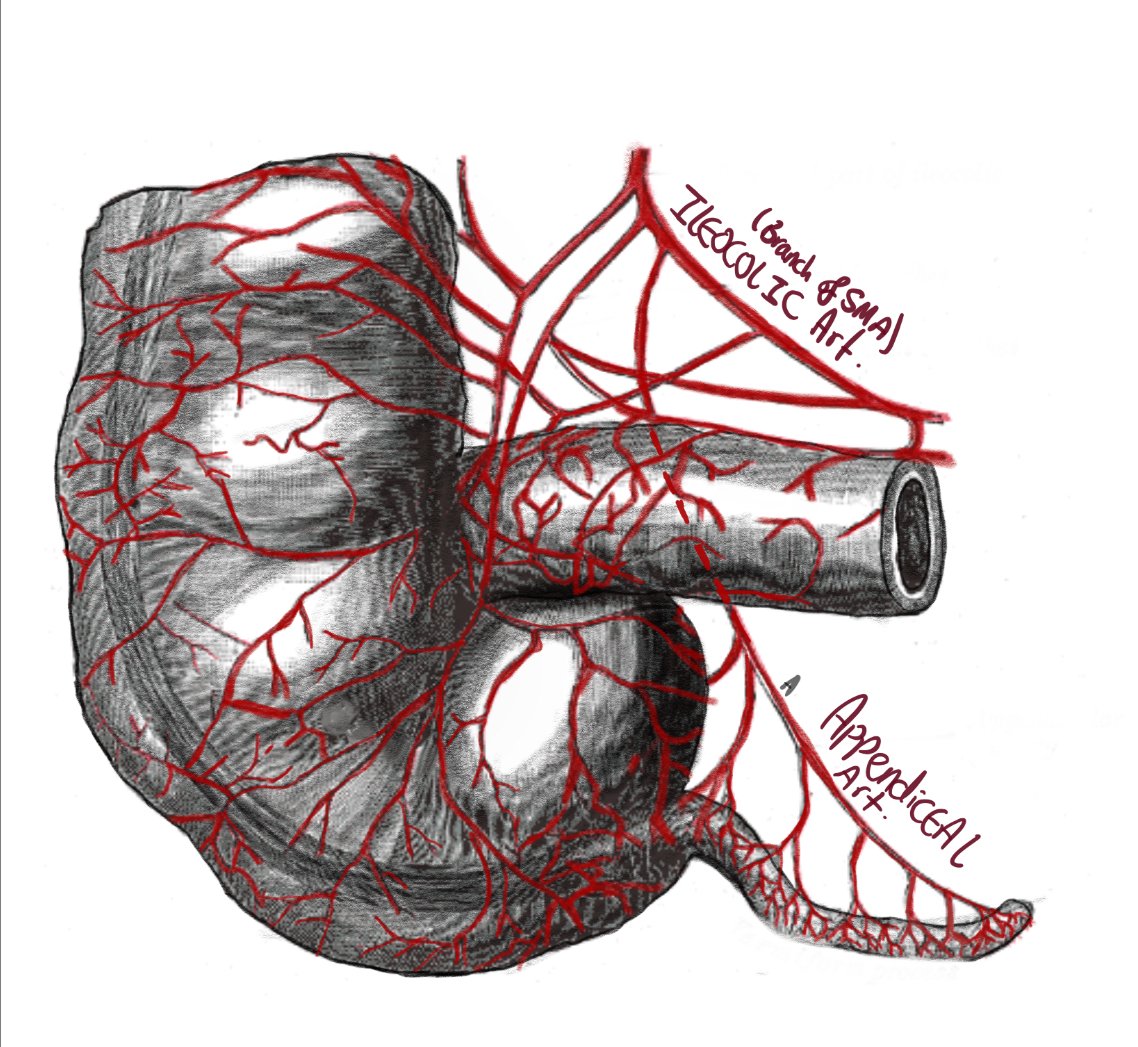
Diagram depicting the ileocolic artery and the appendicular artery supplying the appendix and the terminal ileum.
Clinical Relevance: Appendiceal Perforation vs. Gallbladder Perforation
Why is appendiceal perforation very common in appendicitis, but a perforated gall bladder is a much less common occurrence?
Venous Drainage
Drains into the superior mesenteric vein, which will join the splenic vein forming the portal vein
Lymph Drainage
Nerve Supply
Autonomic innervation
Sensory innervation
Clinical relevance
Introduction
- Appendicitis is one of the most common surgical conditions you will face in general surgery.
- It is the 2nd most common cause of abdominal pain, after non-specific abdominal pain, on the surgical take.
- As a surgeon, an appendicectomy will likely be the first abdominal surgery you will learn to perform.
- The diagnosis of acute appendicitis may generally be seen as an easy diagnosis to make, but it is an exceedingly difficult diagnosis to rule out.
- In clinical practice, you will be surprised how diverse the presentations for acute appendicitis can be.
Definition
Appendicitis is defined as inflammation of the vermiform appendix.
Incidence
The lifetime incidence of acute appendicitis is 8.6% in males and 6.7% in females.
Gender Distribution
- Note there is a slight preponderance of acute appendicitis in males compared to females.
- Females are more likely to undergo a negative appendicectomy (38.5% versus 6.2% in males in some studies).
Age Distribution
- Appendicitis can occur at any age!!
- Most commonly observed in age range of 5-45 yo.
- The mean age of presentation is 26.
- It is mostly a disease of childhood, adolescence.
Clinically relevant anatomy
- The appendix is a blind true diverticulum of the colon.
- It extends from the posterior aspect of the cecum towards the RIF.
- Found laparoscopically in the RIF, at the point where the taenia coli of the ascending colon converge.
McBurney’s point:
- A point found 2/3 of the length of a line drawn from the umbilicus to the right ASIS. Pain at palpation of this point makes a patient “McBurney’s positive.”
- Most appendices will lie retrocecally (65% of the time).
- An appendix with a diameter of over 6mm or a wall thickness of over 3mm is considered thickened and pathological.

description
Appendicular neurovascular supply
- It is supplied by the Appendiceal artery, a branch of the Ileocolic artery which is a branch of the SMA.
Nerve supply
- Pain from appendicitis typically presents as a vague paraumbilical pain which localises to the RIF.
- Pain at paraumbilicus: felt there as the appendix is supplied by sensory fibres that enter thespinal cord at level of T10 (T10 dermatome is the umbilicus).
- pain at the RIF: this is felt when the inflammation worsens and starts irritating the parietal peritoneum of the posterior abdominal wall.
Appendicitis Pain Patterns
Initial Pain
- Pain from appendicitis typically presents as a vague paraumbilical pain.
- It is felt there as the appendix is supplied by sensory fibres that enter the spinal cord at level of T10 (T10 dermatome is the umbilicus).
Pain Localization
- The pain later localises to the right iliac fossa (RIF) as the parietal peritoneum becomes involved.
- Pain at the RIF is felt when the inflammation worsens and starts irritating the parietal peritoneum of the posterior abdominal wall.
Pathophysiology of Acute Appendicitis
Obstruction of the Appendiceal Lumen
The initial cause of acute appendicitis is typically obstruction of the appendiceal lumen. This can be due to various factors such as lymphoid hyperplasia, faecoliths, tumours, or infections.
- Lymphoid Hyperplasia
- Faecoliths
- Hardened masses of stool that can obstruct the lumen. Components include fats (coprosterols), inorganic salts (calcium phosphates), and organic residues (vegetable matter).
- Tumors
- More common in older adults. Neuroendocrine tumours account for about 50% of appendiceal tumors. Mucocele, a swelling or sac filled with mucus, can be benign (cystadenoma) or malignant (cystadenocarcinoma).
Common in younger patients, caused by an increase in lymphoid tissue.
Mucus Build-up
The obstruction causes a build-up of mucus within the appendix.
Increased Pressure
The build-up of mucus increases the intraluminal pressure.
Occlusion of Veins and Lymphatics
The increased pressure occludes the veins and lymphatic vessels, causing congestion and oedema.
Interruption of Arterial Supply
Continued pressure interrupts the arterial blood supply, leading to ischaemia and necrosis of the appendiceal wall.
Bacterial Infection
Bacteria from the colon invade the necrotic wall, leading to infection and further inflammation.
Abscess or Phlegmon Formation
The infection can result in localised abscess formation or a phlegmon (an inflamed mass of tissue).
Full Wall Necrosis
If untreated, full-thickness necrosis occurs, causing perforation and spillage of appendiceal contents into the abdomen.
Peritonitis and Sepsis
The spillage leads to generalised peritonitis and can progress to septic shock if not promptly treated.
Clinical Presentation: Symptoms

Pain
Pain typically starts in the paraumbilical region.
Later localises to the right iliac fossa (RIF) as the parietal peritoneum becomes involved.

Anorexia
Very common in appendicitis.
Appendicitis patients are rarely hungry or willing to eat.
A good question to ask when taking a history from an appendicitis patient is "What's your favorite food?" and "If I could get you that now would you eat it?"

Vomiting
Usually follows the onset of pain and is not a prominent initial symptom.

Diarrhea and Fever
Diarrhea can occur in some patients; if this is the prominent initial symptom, think colitis or enteritis.
Fever is usually low-grade; high fever may suggest mesenteric adenitis or other complications.
Clinical Presentation: Examination Findings
Tenderness
Maximal at McBurney's point, one-third of the distance from the anterior superior iliac spine (ASIS) to the umbilicus.
Rebound Tenderness
Indicates peritoneal irritation.
Guarding
Voluntary or involuntary muscle contraction in response to peritoneal inflammation.
Percussion Tenderness
Pain upon gentle tapping of the RIF.
RIF Mass
May indicate an appendiceal abscess.

Image depicting Mcburney's line and McBurney's point
McBurney's Sign
Maximal tenderness at McBurney's point.
Rovsing Sign
Pain in the RIF upon palpation of the left iliac fossa (LIF), due to peritoneal stretch.
Psoas Sign
Pain on extending the right hip, indicating retrocaecal appendicitis.
Dunphy's Sign
Increased pain in the RIF with coughing.
Differential Diagnosis:
GI Causes
Inflammatory Bowel Disease (IBD)
Can present with RIF pain. Remember the most common site for Crohn's disease is the terminal ileum (which is also in the RIF). Patient will most likely have a preceding history of loose stools, PR bleeding and PR mucus. A short sudden history of RIF pain makes this unlikely (but not impossible).
Meckel's Diverticulum
Meckel's diverticulitis is a complication of Meckel's diverticulum, can have a very similar presentation to appendicitis. It's the commonest congenital malformation of the small bowel. Pathology: True diverticulum of the ileum, forms due to failure to obliterate the vitelinointestinal duct during the 5th week of fetal development.
Diverticulitis
Patients with right-sided diverticulitis tend to be younger than those with left-sided disease and often are misdiagnosed with acute appendicitis. CT scans will differentiate this from appendicitis.
Gynaecological Causes
Mittelschmerz Pain
Refers to midcycle pain in an ovulatory woman caused by normal follicular enlargement. Pain typically mild and unilateral, around midpoint of menstrual cycle.
Ovarian Cyst
Can cause pain similar to appendicitis.
Ectopic Pregnancy
Positive pregnancy test, septic, hypovolemic shock.
Endometriosis
Chronic history, short history and sudden onset pain makes this less likely.
Ovarian Torsion
Can present with acute abdominal pain.
Pelvic Inflammatory Disease
Important to take a full sexual history to discern patients who are most at risk of STIs. Ask about vaginal discharge. Can progress into tuboovarian abscess and involve bladder/bowel.
Urological Causes
Renal Colic
Loin to groin pain classically. Severe pain, patient will be unable to sit still, in severe pain. NOTE: a positive urine dip for blood, leukocytes doesn't rule out appendicitis. A retrocecal appendix can present with a positive urine dip and loin pain.
Urinary Tract Infection (UTI)
Dysuria, off smell to urine, pain not localised to RIF.
Pyelonephritis
Can present with flank pain and fever.
Testicular Torsion
Acute scrotal pain that can be confused with appendicitis.
Epididymorchitis
Inflammation of the epididymis and testicle that can mimic appendicitis.
Pediatric Causes
Mesenteric adenitis
- Refers to inflamed abdominal lymph nodes. This presents with abdominal pain in younger children.
- Usually preceded by or associated with tonsillitis or an upper respiratory tract infection.
- Fevers tend to be high grade (39°C or above) compared to lower grade fevers in appendicitis.
- The condition is self-limiting.
Diagnosis: Imaging - Ultrasound (USS)
Purpose
To visualise a distended appendix and rule out gynaecological causes of RIF pain.
Diagnostic features on USS
Maximal Outer Diameter (MOD)
Refers to the diameter of the appendix. Defined on ultrasound as the distance between the outer hyper echoic borders of the appendix. Over 6mm is considered pathological.
Maximal Mural Thickness (MMT)
The thickness of the appendiceal wall. Defined as the distance from the hyper echoic luminal interface to the outer hyper echoic border. Over 3mm is considered pathological.
Free Fluid
Presence of free fluid in the abdomen is also to be noted. Free fluid in females may be physiological or pathological. In males it is always pathological and raises concern for a perforated hollow viscus.

(A) Long axis view through the right lower quadrant demonstrates a non-compressible, enlarged, fluid-filled blind-ending appendix (arrow).
(B) Short axis scan shows a target appearance characterised by a fluid-filled center, sub adjacent layer of hyper echoic mucosa, and outer layer of hypo echoic muscle (arrow)

Acute appendicitis with an appendicolith. Long axis view shows an enlarged, fluid-filled appendix (A) with an echogenic appendicolith (arrow). Note the acoustic shadowing (arrowhead) caused by the appendicolith
Diagnosis: Imaging - CT Scan
Purpose
Provides detailed imaging and helps confirm the diagnosis of appendicitis.
Diagnostic features on CT scan
Appendix Diameter
Appendix diameter over 6 mm is considered abnormal.
Wall Thickness
Appendiceal wall thickness over 3 mm (target sign) indicates inflammation.
Periappendiceal Inflammation
Fat stranding around the appendix is a sign of inflammation.
Faecolith
Presence of a faecolith can be seen on CT.
Cecal Changes
Thickened cecum funnelling contrast into the appendix can be observed.

CT scans in a 53-year-old man with abdominal pain. Transverse CT scans (A, B) and coronal reformation (C, D) obtained with intravenous contrast material show the thickened appendix (arrows) and oedema in cecum (arrowheads) at the orifice of the appendix. At surgery, an inflamed appendix was identified and removed.
Diagnosis: Laboratory Tests - Blood Tests
White Blood Cell Count (WBC)
A rise in neutrophils indicates infection and inflammation.
C-Reactive Protein (CRP)
Elevated levels suggest inflammation, but normal levels do not rule out appendicitis.
Bilirubin
Elevated levels may indicate perforation.
Diagnosis: Laboratory Tests - Urine Tests
Urine Dipstick
To rule out urinary tract infections (UTI) as a cause of the pain. Presence of leukocytes, blood, and nitrites can be seen in retrocolic appendicitis due to ureteric irritation.
Beta-HCG
Essential for ruling out pregnancy and ectopic pregnancy in women of childbearing age, which is crucial before performing surgery or imaging involving radiation.
Management of Acute Appendicitis: Initial Management
Patient Assessment
- Patients may be unwell and septic on presentation.
- Use principles of sepsis 6 and CCRISP protocol to manage the patient.
Early Interventions
- Early administration of antibiotics and IV fluids is important.
- Insert a urinary catheter to guide fluid prescribing and resuscitation.
Preparation for Surgery
- Patient to be made nil by mouth (NBM) from time of assessment to fast for potential surgery.
Pain Management
Pain management should ensure patients are kept comfortable.
Monitoring
Input-output accurate measurement is essential to prevent acute kidney injuries, dehydration, and electrolyte disturbances.
Management of Acute Appendicitis: Definitive Management
Non-operative Management
- a potential management plan, especially in elderly patients, patients unfit for surgery, patients not agreeable to surgery
- Effective in 70-90% of uncomplicated appendicitis cases. However, there is a high risk of recurrence (15-30%).
- Presence of a faecolith increases risk of complications and recurrence very significantly.
- In older patients, you need to exclude an occult malignancy with a colonoscopy.
Surgical Management
- A laparsocopic appendicectomy is the standard management of acute uncomplicated appendicitis.
- For details notes on laparoscopic appendicectomy, scroll to the top and use the surgical view tab.
Management of Complicated Appendicitis
The natural progression of appendicitis, if left untreated, can result in various outcomes:
- Resolution
In rare cases, the inflammation may subside on its own.
- Generalized Peritonitis
- If the appendix undergoes necrosis, it may lead to a large perforation.
- This perforation can cause the release of infectious material into the abdominal cavity, resulting in generalized peritonitis—a severe and life-threatening condition.
- Appendix Mass or Phlegmon Formation
- The inflamed appendix may become surrounded by omentum and adjacent small bowel.
- This forms a protective barrier, or "walling-off," that confines the inflammatory process and prevents it from spreading to the rest of the abdominal cavity.
- Appendiceal Abscess
- An abscess may develop in the periappendiceal region, encapsulating the infection within a localized, walled-off area.
Management strategy is different in complicated appendicitis as presence of an abscess or a phlegmon increases risk of surgical complications.
Management of generalized peritonitis
Should be operated on to control the source of sepsis, washout, drain insertion
Management of perforated appendix causing phlegmon
- Managed non-operatively with abx with or without interval appendicectomy.
- Failure rate of abx only is 7%
- Risk of recurrence 7-40%
- Risk of important benign disease being missed is 7%.
Managed operatively with immediate appendicectomy.
- No risk of recurrence of appendicitis
- HIGH RISK OF COMPLICATIONS: due to severe surrounding inflammation and adhesions.
- 20% may need cecectomy
- 30% may need ileocolectomy.
Therefore, an initially nonoperative approach, with subsequent interval appendectomy is certainly a reasonable strategy,
- The role for a subsequent interval appendicectomy is debatable.
- A large systematic review showed
Appendiceal abscess management
- These are generally diagnosed preoperatively because imaging is now a routine part of the diagnostic process.
- Abscess will form in one of the following locations:
- right paracolic gutter
- subcecal area
- pelvis
- There are three general approaches management:
- Percutaneous drainage with interval appendectomy
- Percutaneous drainage without appendectomy,
- Immediate operative drainage and appendectomy.
- higher risk of requiring a further resection (same as phlegmons).
Post operative complications
Hospital stay:
- Full diet and early mobilisation is recommended as soon as possible post-op
- most patients who are comorbidity free can be discharged within 24 hours of an appendicectomy
- prolonged hospital stay is more common in patients with other comorbidities, or those frail and unlikely to return to their premorbid state, requiring care arrangements on discharge.
Wound infection
- The commonest post operative complication of an acute appendicectomy
- less common in patients done laparoscopically compared to patients done open.
- wound is usually superficial requiring a course of oral abx.
- deeper infections may lead to dehisence of the wound. Management of this may require washout of wound, drainage of any associated soft tissue abscess and prolonged dressings.
Collection formation
- pericaecal fluid collections are relatively common
5-10 days post op
- present with post-op discomfort and low grade pyrexia—> collection
- swinging pyrexia and pain—> abscess.
- management of both is IR guided drainage and prolonged course of iv abx. Surgical washout maybe indicated in patients who are in shock, or those who dont respond to conervative management.
first 48 hours post op
- fevers, pain, septic shock, peritonism in the first 24 hours may indicate dissemination of infected fluid or inappropriate washout of purulent fluid.
- The main differential diagnosis is iatrogenic injury to small bowel during port zinsertion or otherwise intraoperatively.
- early washout and diagnostic laparoscopy is recommended in those patients.
Appendicitis (Surgeon's view)

This page will provide a comprehensive overview of the laparoscopic appendectomy procedure, from patient consent to surgical technique and postoperative care.
Patient Consent: Understanding the Procedure
Incisions
Brief explanation:
- 3 small cuts in abdomen.
- long camera and instruments used
- appendix removed
Conversion
- may be converted to open if surgery complicated, difficult or unsafe to perform lapoaroscopically, larger incision used, more pain, slower recovery
- I like to use the diagram below to explain lap converted to open

Diagram to show patients the conversion from lap to open
Risks Associated with Surgery
Bleeding
- Due to large vessel injury including aorta
- Due to bleeding when inserting LIF port from left inferior epigastric vessel.
Injury to surrounding structures
- Damage during laparoscopic assessment or port insertion
- Including fallopian tubes, bowels, ureters, bladder
Scarring and wound complications
- as with any surgery, the way the wound will heal is unpredictable, may leave a noticeable scar
- wound infection due to inherently dirty surgery (involves infected structure)
Conversion to open surgery
- Difficult procedure
- Other pathology such as carcinoid tumour
Damage during port insertion
- Bowel: may lead to stoma formation
- Bladder (during suprapubic port)
- Ask patient to pass urine pre op or insert a catheter (in and out during anaesthetic).
Removal of ovary or Fallopian tube
- Not in an appendectomy
- In case of tubovarian pathology.
Collection
- Appendix is inherently dirty
- Collection may require a drain or more abx.
- More likely with a perforation
Conversion to open surgery
- Difficult procedure
- Other pathology such as carcinoid tumour
Laparoscopic appendicectomy
Cost issues
- This has now considered the gold standard for an appendicectomy in adult patients.
- Due to increased cost of equipment associated with laparoscopy, open appendicectomy has remained the standard practice in some developing countries.
Compared to open:
- Multiple meta-analyses confirmed(1) (2)
- benefits including:
- faster recovery
- smaller scars
- lower incidence of wound infection
- Risks including:
- 3x increase in risk of post op collection
- longer opening time (16 minutes longer on average)
- benefits including:
Pre-operative Patient Preparation
Patient Positioning
Place the patient supine with the right arm out and left arm in.
Catheterization
- catheter to empty bladder and make suprapubic port incision easier.
- some surgeons use it routinely, others will ask patient to pass urine pre-op and avoid inserting a catheter.
Additional Preparations
- TED stocking on, if prolonged procedure anticipated, consider flautrons
- Electrocautery pad on
- Electric shaver+ tape to collect hair.
Post scrubbing in: Surgical Field Preparation
Antiseptic Application
Use 4% chlorhexidine (or follow local guidance) to thoroughly clean the entire abdomen, paying special attention to the umbilicus.
Draping
Carefully drape the surgical field to maintain sterility.
Antibiotic Administration
Ensure prophylactic antibiotics are administered as per protocol.
Surgical Team Positioning
Position the surgeon on the patient's left side and the assistant on the right initially, with the assistant moving to the left after port insertion.
Port Placement for Laparoscopic Appendectomy
| Port | Size | Insertion Technique | Use |
|---|---|---|---|
| Umbilical | 5-12mm | Modified Hasson | Camera port |
| LIF | 5mm | Under direct vision | Right hand instrument |
| Suprapubic | 5mm | Under direct vision | Left hand instrument |
First Port Insertion: Modified Hasson Technique
Incision
- Grasp the umbilical stalk with a littlewoods forceps.
- Make an infraumbilical or supraumbilical transverse curved incision using a size 11 blade.
Dissection
Peritoneal Entry
Make a vertical midline incision at the junction of the umbilical stump and linea alba.
Port Insertion
Insert a blunt trocar, pointing away from major vessels, and establish pneumoperitoneum.
Establishing Pneumoperitoneum
Insufflation
Insufflate the abdomen to create a working space for the procedure.
Pressure Maintenance
Maintain intra-abdominal pressure between 12-15 mmHg using high flow.
Monitoring
Be prepared to release pneumoperitoneum if the anesthesiologist reports ventilation difficulties or reduced venous return.
Insertion of Secondary Ports
LIF Port
- 2 fingerbreadths superior and medial to the left ASIS
- You need to avoid injury to left inferior epigastric vessels
- shine camera into peritoneum internally, you should see epigastric vessels
- go medially or laterally to them
Suprapubic Port
- inserted to triangulate with 2 other ports.
- ensure bladder is not going to be injured.
- if this is challenging perform a trendelenberg manouver to get small bowel out of the way.
Visualization
- Use camera guidance to ensure safe insertion of both secondary ports.
- Position the patient in Trendelenberg position to allow small bowel to move to the superior part of the abdomen with gravity to ease visualisation of the appendix.

Diagram depicting the Trendelenberg and reverse Tendelenberg positions
Diagnostic Laparoscopy
Thorough Examination
Assess the gallbladder, large bowel, small bowel, and in females, examine the ovaries.
Normal Appendix?
If the appendix appears normal, examine the terminal ileum for Meckel's diverticulum.
Washout
- Aspirate any purulent fluid for microbiology and perform a washout.
- this is to avoid contaminating further quandrants of the abdomen when you perform a steep trendelenberg later
Documentation
Record all findings for accurate post-operative reporting and follow-up.
Locating the Appendix
Teniae Coli Guidance
Follow the convergence of the three thickened bands of longitudinal muscles (teniae coli) to find the appendix base.
Appendix Manipulation
Once found, grasp the appendix with the left hand and pull it anteriorly, laterally, and caudally to visualize the mesoappendix.
Reach the base of the appendix
- Use a combination of blunt and sharp dissection to reach the base of the appendix.
- This allows complete resection of the appendix
- remember! a subtotal cholecystectomy is a good operation, a subtotal appendicectomy on the other hand isnt!!

Image showing the appendix viewed through a laparoscopic camera. The base of the cecum can be seen.
Dissecting the Mesoappendix
Aim
aim to clear the mesoappendix at the base of the appendix to prepare for ligation of the base.
Window Creation
Use hook diathermy to create a window in the mesoappendix.
Careful Dissection
Dissect through layer by layer, only cutting tissue that is clearly visible to avoid vessel injury.
Vessel Management
Cauterize the appendiceal artery when identified. Use clips for larger vessels if necessary.
Base Preparation
Clear the mesoappendix at the base to prepare for appendix ligation.

The mesoappendix disected of the appendix.
Resecting the Appendix
Endoloop Placement
Place Vicryl or PDS endoloops at the base of the appendix.
- endoloop in right hand, grasper in left hand
- insert grasper though the endoloop
- grasp appendix tip with left hand and pull it through the loop.
Ligation Technique
Apply two proximal loops close together and one loop 1cm distally.
Appendix Division
Cut the appendix between the loops, leaving two endoloops on the stump and one to keep the appendix closed during removal.
inspect base of the appendix and surrounding area to ensure good haemostasis.
Removing the Appendix
Retrieval Bag Insertion
- Insert a retrieval bag through the umbilical port.
- push bag towards liver to make space
- insert camera throough same port
Appendix Placement
Use two graspers to place the appendix into the bag.
Bag Removal
Carefully pull the bag containing the appendix through the umbilical port.
Appendix Inspection
- inspect the removed specimen, make sure its an appendix *small pouch with a lumen
- you will be surprised sometimes a lump of fat or a lymph node may be mistaken for an appendix!
Peritoneal Washout
Thorough Irrigation
Perform a good washout of the peritoneal cavity until the fluid runs clear.
Pelvic Clearance
Ensure all fluid in the pelvis is cleared to prevent postoperative collections.
Drain Insertion Considerations
Current Evidence
Meta-analyses show drains have no effect on intra-abdominal collections in complicated appendicitis.
Potential Risks
Drains may increase the risk of postoperative complications such as fistula, surgical site infection, bowel obstruction, and ileus.
Decision Making
Consider the individual case and surgeon preference when deciding on drain placement.
Removal of Ports and Closure
Secondary Port Removal
Remove LIF and suprapubic ports under direct vision, ensuring no bleeding on deflating pneumoperitoneum.
Umbilical Port Closure
Close the umbilical port with J PDS or J Vicryl suture.
- insert finger into the defect, pull the suture upwards closing the defect on finger.
- Close the defect fully while ensuring no bowel is caught in the closing suture
- tie the suture to close the defect.
- inspect and feel after tying the stitch to ensure defect successfully closed
Skin Closure
Close all skin incisions with 3/0 Monocryl sutures.
Final Inspection
Perform a final check of all incision sites to ensure proper closure and hemostasis.
Hints and Tips for Successful Laparoscopic Appendectomy
Maintain Traction
Keep appropriate traction on the appendix throughout the procedure for better visualization and dissection.
Camera Flexibility
Using a 5mm laparoscopic camera allows for insertion through different ports, increasing maneuverability.
Safe Diathermy
When using the diathermy hook, dissect towards the anterior abdominal wall to avoid injuring surrounding structures if you overshoot.
Ask for Help
If not progressing, consider asking for help or converting to open procedure early, before fatigue sets in.
Pitfalls to Avoid in Laparoscopic Appendectomy
Misidentification
Ensure confident identification of the appendix to avoid removing other structures like fallopian tubes or ovaries.
Ureter Injury
Be conscious of the ureter's proximity, especially when the retroperitoneum is friable and inflamed.
Incomplete Hemostasis
Always leave a dry field to prevent postoperative complications.
Inadequate Visualization
Maintain proper camera positioning and cleaning to ensure clear view throughout the procedure.
Open Appendectomy: Patient Positioning
Patient Position
Position the patient supine, preferably with arms tucked in at the sides.
Surgeon Position
The surgeon stands on the right side of the patient.
Assistant Position
The assistant stands on the left side of the patient.
Open Appendectomy: Incision and Exposure
Incision Choice
Choose between McBurney's/Grid iron incision or Lanz incision based on surgeon preference.
- McBurney’s/Grid iron incision:
- an incision perpendicular to the line that forms McBurney’s point.
- how to locate
- find Mc Burney’s line (a line between ASIS and the umbilicus).
- how to locate
- an incision perpendicular to the line that forms McBurney’s point.

Diagram depicting McBurney's point
- Find McBurney’s point (a point 1/3 from the ASIS on this line)

Diargram depicting McBurney's point
- Gridiron incision: Draw a line perpendicular to McBurney’s line, bisecting McBurney’s line at Mc Burney’s point.

Gridiron incision
- Lanz incision
- a line through McBurney’s point.
- More transverse in comparison to the Gridiron incision (try to follow the skin creases)
- follow’s langer’s lines more closely, better. cosemsis

Lanz incision
Layer Dissection
- Divide the subcutaneous fat and the scarpa’s fascia until you reach the external oblique aponeurosis.
- apply a self retaining retractor to free your assistant
Layers you will find will be as follows:
Skin
Camper's Fascia
Scarpa’s fascia
External oblique
Internal oblique
Transversus abdominis
Transversalis fascia
Peritoneum
Muscle Splitting
Split muscle layers parallel to their fibers to minimize postoperative pain and risk of incisional hernias.
Peritoneal Entry
Enter the peritoneum carefully, watching for adherent bowel.
Dividing muscle layers
External oblique
- raise the external oblique aponeurosis with 2 mosquito clips
- open aponeurosis with a knife cutting between your mosquito clips PARALLEL TO THE MUSCLE FIBRES
- extend the incision with tissue scissors along the length of the wound (making sure you use the full length of you incision to get as much space as you can with the available wound).
Internal oblique
- split the layer with a pair of mayo scissors PARALLEL TO MUSCLE FIBRES
- Layer is pulled apart by 2 langenbeck retractors by your assistant.
Transversalis fascia
- two mosquito clips are applied to tent the fascia upwards
- ensure no bowel is cause in the clip
- make a small cut with dissecting scissors. Extend this along the length of the incision.
Peritoneum
- preperitoneal fat is dissected and the peritoneum is held with 2 mosquito clips.
- the perioneum is lifted and a small cut is made with scissors. Extend this along the length of the wound.
Open Appendectomy: Finding and Removing the Appendix
Appendix Localization
Use the anatomical landmarks described above to locate the appendix at the base of the cecum.
Mesoappendix Dissection
- once the appendix is found, grasp it with a Babcock Forceps and deliver it through the wound.
- Dissect a window into the mesoappendix with artery clips
- ligate the appendiceal artery with 2/0 vircyl ties (or transfix with 2/0 vircyl sutures
Appendix Removal
- the base of the appendix is crushed with a large crushing clip
- unclip, move the clip distally and apply it again.
- ligate or transfix the base of the appendix with 2/0 vircyl
- divide the appendix with a blade along the proximal end of the curshing forceps in one controlled move.
Burying the appendiceal stump
- use 2/0 vicryl ties to perform a pursestring stitch at base of cecum to bury the base of the appendix into the cecum.
- this is an optional step. Different studies have found this to not make a difference in outcomes.
Open Appendectomy: Closure Method
Peritoneal Closure
Close the peritoneum with continuous 2/0 Vicryl sutures.
Muscle Approximation
Approximate muscles with loose interrupted 2/0 Vicryl sutures.
External Oblique Closure
Close the external oblique aponeurosis with continuous 2/0 Vicryl sutures.
Skin Closure
Close the skin with 3/0 Monocryl sutures or use clips if there is frank contamination.
Managing a Normal Appendix
Alternative Pathology
If another cause for abdominal pain is found, address it and consider leaving the normal appendix in place.
No Obvious Cause
If no other cause is found, it's generally advised to remove the appendix to prevent future diagnostic uncertainty.
Considerations
Weigh the risks of unnecessary surgery against the potential for future complications or diagnostic challenges.